Wisconsin’s Department of Health Services (DHS) and Department of Public Instruction (DPI) are rolling out significant updates to Medicaid School-Based Services (SBS) that promise to reshape how special education services are delivered and reimbursed. These changes, driven by a state-initiated reversal of the Free Care Rule and new federal mandates from the Centers for Medicare & Medicaid Services (CMS), expand access, streamline compliance, and ensure students receive the support they need.
Latest update:
In December 2025, Wisconsin DPI shared additional finalized guidance related to updates in the Wisconsin SBS program—building on previously announced changes and providing clearer direction for districts moving forward. Key documents include Revisions to Medicaid School-Based Services (SBS) and the Medicaid School-Based Services (SBS) Expansion Overview, which outline what’s changing and what districts should be preparing for next year.
This blog highlights the updates most important to school districts and summarizes the steps they can take to help maximize reimbursement in 2026.
Expanded Access to Medicaid School-Based Services
One of the most transformative changes is the expansion of SBS eligibility. Previously, only students with Individualized Education Programs (IEPs) qualified for Medicaid-covered services in schools. Now, the program includes Medicaid-enrolled students without IEPs, encompassing those with 504 plans, Individual Health Plans, Behavior Intervention Plans, doctor’s orders, or other documentation establishing medical necessity. This broader eligibility has opened doors for more students to access critical services, from speech therapy to mental health support.
The scope of covered services is also growing. New additions include physician services, dental care, targeted case management, and expanded Early Periodic Screening, Diagnostic, and Treatment (EPSDT) services. To deliver these, Wisconsin has introduced new provider types, such as Board-Certified Behavior Analysts and Registered Behavior Technicians, with potential expansions into areas like Applied Behavior Analysis (ABA) therapy. A Medicaid plan of care still remain a prerequisite for most billable services, and documentation requirements will align with those for IEP students, ensuring consistency.
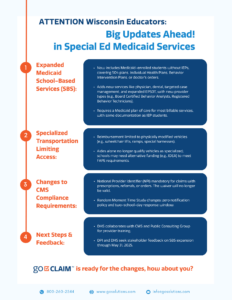
Here’s a quick rundown of what’s new:
- Now includes Medicaid-enrolled students without IEPs, covering 504 plans, Individual Health Plans, Behavior Intervention Plans, or doctor’s orders.
- Adds new services like physician, dental, targeted case management, and expanded EPSDT, with new provider types (e.g., Board Certified Behavior Analysts, Registered Behavior Technicians).
- Requires a Medicaid plan of care for most billable services, with same documentation as IEP students.
Click to view the full infographic on what’s changed in special education Medicaid services across Wisconsin in 2026.
Specialized Transportation: A Shift in Standards
Transportation for students with special needs is another area that received significant updates. CMS has tightened reimbursement criteria, limiting coverage to trips on physically modified vehicles—think wheelchair lifts, ramps, or special harnesses. The presence of an aide no longer qualifies a vehicle as “specialized,” which could impact schools’ budgets. For students whose IEPs include transportation but don’t require modified vehicles, schools may need to tap alternative funding sources, like IDEA grants, to meet Free and Appropriate Public Education (FAPE) obligations. This shift underscores the need for careful planning to ensure compliance and student access.
To sum it up, major updates include:
- Reimbursement limited to physically modified vehicles (e.g., wheelchair lifts, ramps, special harnesses).
- Aides alone no longer qualify vehicles as specialized; schools may need alternative funding (e.g., IDEA) to meet FAPE requirements.
💡 Takeaway for school districts:
Having the right tools and preparation is key. School districts should equip themselves now to maximize Medicaid billing opportunities under Wisconsin’s updated SBS program.
Federal Compliance: NPIs and Time Studies
To align with CMS guidance, Wisconsin has implemented stricter compliance measures. A Type 1 National Provider Identifier (NPI) is now required on claims involving prescriptions, referrals, or orders. DHS and DPI are exploring ways to roll out this requirement smoothly, allowing flexibility in how NPIs are used across providers.
Meanwhile, the Random Moment Time Study process is getting an overhaul. Schools now face a “zero notification” policy, meaning no advance warning before a study moment, and the response window has shrunk from five school days to two. These changes aim to improve accuracy and accountability in how Medicaid funds are allocated.
- National Provider Identifier (NPI) mandatory for claims with prescriptions, referrals, or orders. The waiver will no longer be valid.
- Random Moment Time Study changes: zero notification policy and two-school-day response window.
What’s Next for Wisconsin Schools?
As Wisconsin moves forward, staying informed and engaged will be key. Schools should begin assessing their transportation fleets, training staff on NPI requirements, and preparing for the updated time study process. For families, these changes mean more opportunities for their children to access vital services, regardless of IEP status. Together, these efforts will help ensure Wisconsin’s special education system remains robust, inclusive, and responsive to student needs.
💡 Recommended reading: Factors Affecting Students’ Medicaid Eligibility for School-Based Services
💡 Recommended reading: Ultimate Guide for Medicaid Billing in Wisconsin
Final Thoughts
These changes reflect Wisconsin’s commitment to equitable access to special education services while navigating complex federal requirements. By expanding SBS eligibility and services, more students will benefit from tailored support. However, the transition won’t be without challenges—schools will need to adapt to new transportation rules, comply with tighter CMS mandates, and prepare for increased documentation demands.
Featured Product
Looking for a smarter way to handle school-based Medicaid billing?
GoClaim provides trusted tools and expert support tailored specifically for your school district — so you can simplify compliance, maximize reimbursements, and focus on student services.